Treatments
Diabetic Retinopathy
Diabetic Eye Disease
Diabetes can affect mostly all parts of the eye but the most serious complications occur when it affects the retina (the seeing part of the eye which is situated at the back end of the eye ball).
Diabetic Retinopathy is caused when diabetes affects the small blood vessels which carry nutrients to the retina.
Normal Retina of
Right Eye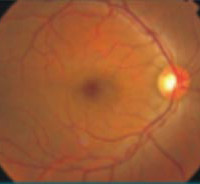
Normal Retina of
Left Eye
-
Normal Angiogram
(FFA) of RE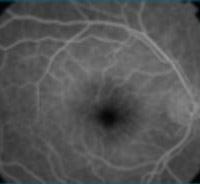
-
Normal Angiogram
(FFA) of LE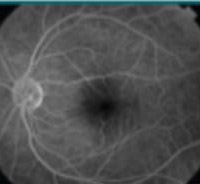
Damage to the retina is of two types:
There may be small leaks from the blood vessels causing bleeding or exudation:
Early Bleeding 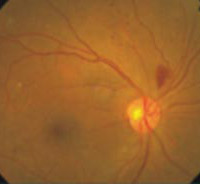
Exudations 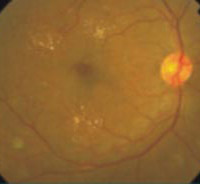
-
Retinal Bleed
and exudates
-
FFA of the
leakages (White color)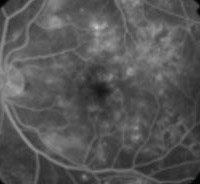
There may be small blockages (occlusions) stopping blood from flowing to one part of the retina
Colour Photo
of occlusion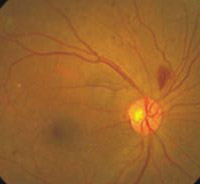
FFA - dark areas with
no blood flow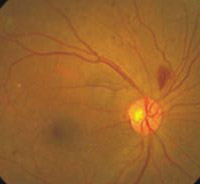
Diabetic Eye Exam
When to do an eye test?
First retinal exam should be immediately upon diagnosis of diabetes as the eye surgeons can record what the normal appearance of the retina is, and also find out any early damage.
Next eye exams will depend on the report of the first exam.
- If damage is not evident : every year
- If mild retinopathy : every six months
- If severe retinopathy : every 3 months
- If laser has been done: every 3 months
- If surgery has been done: every 2 months
Investigations
- Blood Sugar FBS/PPBS
- Cholesterol (Lipid profile)
- High Triglycerides cause pancreatitis damaging the pancreas which is responsible for insulin production.
- HbA1C- helps the surgeon to determine the level of diabetes control over the last three months.
- Renal function test (Blood Urea, Serum creatinine, Albumin)
Recommended Sugar Levels
- FBS < 110 PPBS < 150
- BP < 130/85 mm Hg
Surgical Procedures in Diabetic Retinopathy
- The usual procedures are
- Injection of Triamcinalone
- Injection of Anti-VEGF factors
- Vitreous Surgery
